771 0 comments
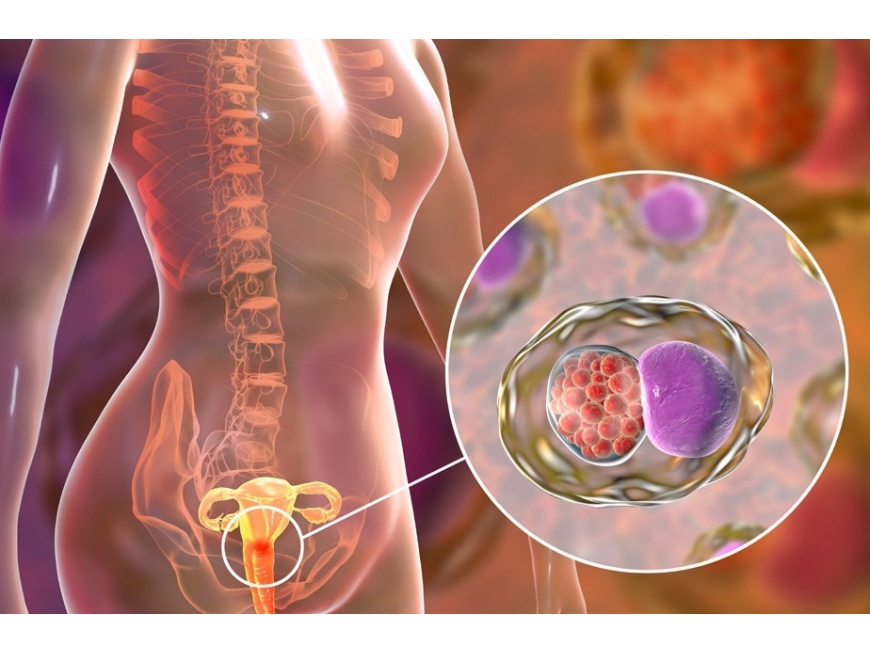
Cervical cancer develops in a woman's cervix (the entrance to the uterus from the vagina).
Almost all cervical cancer cases (99%) are linked to infection with high-risk human papillomaviruses (HPV), an extremely common virus transmitted through sexual contact.
Although most infections with HPV resolve spontaneously and cause no symptoms, persistent infection can cause cervical cancer in women.
Cervical cancer is the fourth most common cancer in women. In 2018, an estimated 570 000 women were diagnosed with cervical cancer worldwide and about 311 000 women died from the disease.
Effective primary (HPV vaccination) and secondary prevention approaches (screening for, and treating precancerous lesions) will prevent most cervical cancer cases.
When diagnosed, cervical cancer is one of the most successfully treatable forms of cancer, as long as it is detected early and managed effectively.
Cancers diagnosed in late stages can also be controlled with appropriate treatment and palliative care.
With a comprehensive approach to prevent, screen and treat, cervical cancer can be eliminated as a public health problem within a generation.
Cervical cancer is cancer that starts in the cells of the cervix. The cervix is the lower, narrow end of the uterus (womb). The cervix connects the uterus to the vagina (birth canal). Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which abnormal cells begin to appear in the cervical tissue. Over time, if not destroyed or removed, the abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and to surrounding areas.
The cervix has two main parts:
* The ectocervix (also called exocervix) is the outer part of the cervix that can be seen during a gynecologic exam. The ectocervix is covered with thin, flat cells called squamous cells.
* The endocervix is the inner part of the cervix that forms a canal that connects the vagina to the uterus. The endocervix is covered with column-shaped glandular cells that make mucus.
The transformation zone is the border where the endocervix and ectocervix meet. Most cervical cancers begin in the squamous cells in the transformation zone.
Types of cervical cancer
Cervical cancers are named after the type of cell where the cancer started. The two main types are:
* Squamous cell carcinoma: Most cervical cancers (up to 90%) are squamous cell carcinomas. These cancers develop from cells in the ectocervix.
* Adenocarcinoma: Cervical adenocarcinomas develop in the glandular cells of the endocervix. Clear cell adenocarcinoma, also called clear cell carcinoma or mesonephroma, is a rare type of cervical adenocarcinoma.
Sometimes, cervical cancer has features of both squamous cell carcinoma and adenocarcinoma. This is called mixed carcinoma or adenosquamous carcinoma. Very rarely, cancer develops in other cells in the cervix.
Cervical cancer risk factors
Risk factors for cervical cancer include:
* Many sexual partners. The greater your number of sexual partners — and the greater your partner's number of sexual partners — the greater your chance of acquiring HPV.
* Early sexual activity. Having sex at an early age increases your risk of HPV.
* Other sexually transmitted infections (STIs). Having other STIs — such as chlamydia, gonorrhea, syphilis and HIV/AIDS — increases your risk of HPV.
* A weakened immune system. You may be more likely to develop cervical cancer if your immune system is weakened by another health condition and you have HPV.
* Smoking. Smoking is associated with squamous cell cervical cancer.
* Exposure to miscarriage prevention drug. If your mother took a drug called diethylstilbestrol (DES) while pregnant in the 1950s, you may have an increased risk of a certain type of cervical cancer called clear cell adenocarcinoma.
PREVENTION
To reduce your risk of cervical cancer:
* Ask your doctor about the HPV vaccine. Receiving a vaccination to prevent HPV infection may reduce your risk of cervical cancer and other HPV-related cancers. Ask your doctor whether an HPV vaccine is appropriate for you.
* Have routine Pap tests. Pap tests can detect precancerous conditions of the cervix, so they can be monitored or treated in order to prevent cervical cancer. Most medical organizations suggest beginning routine Pap tests at age 21 and repeating them every few years.
* Practice safe sex. Reduce your risk of cervical cancer by taking measures to prevent sexually transmitted infections, such as using a condom every time you have sex and limiting the number of sexual partners you have.
* Don't smoke. If you don't smoke, don't start. If you do smoke, talk to your doctor about strategies to help you quit.
Female health (7)
Healthy life style (14)






-100x125.jpeg)
-100x125.jpeg)
-100x125.jpeg)

-100x125.jpeg)
-100x125.jpeg)
-100x125.jpeg)
Write a comment